Major Depressive disorder (MDD)

What is Major Depressive Disorder (MDD)?
Major depressive disorder is common and disabling
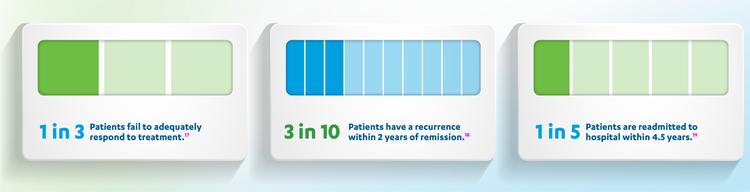
MDD (also known as major depressive disorder) is characterised by prolonged and clinically significant symptoms of depression that are not clearly caused by another medical condition. With a lifetime prevalence of 3–21%, the various sub-types of MDD are associated with significant morbidity, disability and mortality, including an increased risk of suicide. The wider societal impact of MDD is also considerable, with a reduced ability to work and be productive. Therapeutic approaches include pharmacological and non-pharmacological treatments, although up to 3 in 10 patients fail to respond to treatment and are considered treatment resistant (fail to respond to two or more antidepressants during a single episode of major depression).

The prevelance of MDD is 10-20%
According to WHO 2015 estimates, over 40 million people suffer with depression in Europe.A 2020 systematic review on the prevalence of MDD revealed a lifetime prevalence among adults of between 3-21% in Europe. This included data from 38 surveys conducted in 29 countries worldwide and showed that Europe had the highest regional average lifetime and 12-month prevalence (11.32% and 5.2%, respectively).
Lifetime prevalence of MDD in Europe
Country | Lifetime Prevalence (%) |
|---|---|
Country Belgium | Lifetime Prevalence (%) 14.1 ± 1.0 |
Country France | Lifetime Prevalence (%) 21.0 ± 1.1 |
Country Germany | Lifetime Prevalence (%) 9.9 ± 0.6 |
Country Italy | Lifetime Prevalence (%) 9.9 ± 0.5 |
Country Netherlands | Lifetime Prevalence (%) 17.9 ± 1.0 |
Country Spain | Lifetime Prevalence (%) 10.6 ± 0.6 |

Symptoms of MDD
The symptoms of major depression impair an individual's ability to perform normal daily functions at home and at work. Symptoms include:






A large cross-sectional study involving 2,811 adult patients experiencing a major depressive episode established the following symptom frequency;







Plus, suicide risk is significantly elevated among patients with major depression.
A survey conducted in Italy on 324 patients with major depression and their relatives found:



Note: these data refer to a mixed population of both patients and carers – separate data for each group was not made available
To learn more about the impact MDD can have on patients and those around them, visit the 'Quality of Life' page
Classification of MDD
Depressive disorders are classified according to the 2013 Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) or the International Classification of Diseases, 10th Revision (ICD-10) classification of mental and behavioural disorders. An update to the ICD has been developed (ICD-11), but global uptake and implementation is still underway.
Prognosis of MDD
MDD often follows a chronic course, first conceptualised in 1991 by the MacArthur Foundation Research Network on the Psychobiology of Depression task force. On average, a patient faces just under 4 lifetime episodes, with the longest episode lasting 26 weeks.
MDD relapse and recurrence
Consensus definitions of key stages and outcomes in MDD were developed, and revised in 2006, with more recent evidence-based modifications published in 2019
2019 Consensus definitions
Key stage | Definition | Timeframe |
|---|---|---|
Key stage MDD episode | Definition Symptoms meet DSM-5 / ICD-10 criteria | Timeframe ≥ 2 weeks |
Key stage MDD episode remission | Definition A less symptomatic state HAMD-17 ≤ 4 | Timeframe |
Key stage MDD recurrence | Definition A new period of MDD symptoms | Timeframe |

Causes of MDD
MDD is a complex disorder that results from a combination of several genetic factors and environmental influences. Studies have identified the following factors to be associated with MDD, which include but are not limited to:




The COVID-19 pandemic has caused a decline in mental wellbeing among all age groups in Europe, especially among those who have lost their jobs.
Risk of depression by age group and e-survey round, EU27 (%)
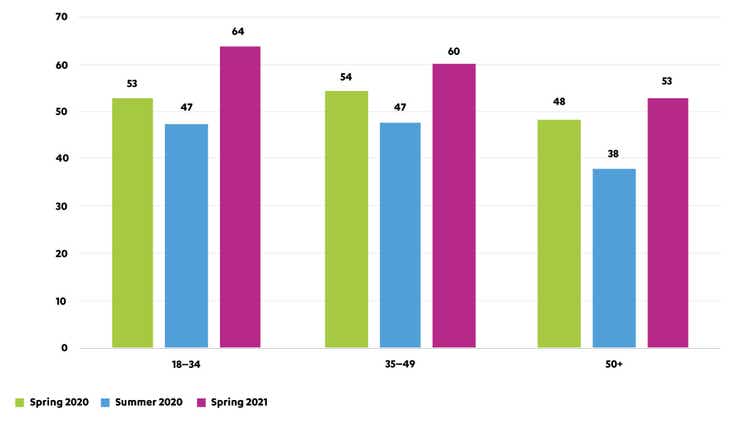
Note: Based on WHO-5 mental well-being index. People with a WHO-5 score of 50 or lower are considered to be at risk of depression
Chart adapted from Eurofound
To learn more about the causes of depression visit the ‘Causes of MDD' page
Impact of MDD
WHO reports that mental health is a leading cause of disability worldwide.
Compared to the general population, patients with MDD have significantly greater rates of:




Comorbidities and MDD

Studies have consistently shown a strong correlation between physical comorbidities and MDD.
The World Health survey found between 9-23% of participants across 60 countries with one or more chronic physical disease had comorbid depression.
The World Health survey found there was a significant association between depression and:




Plus, patients with depression are more than 1.5 times likely to develop ischaemic heart disease than the general population.

Subtypes of major depression/MDD
Subtypes of MDD include postpartum and antepartum depression, psychotic depression and seasonal affective disorder.
Patients with other mental health conditions may also experience depressive symptoms but do not necessarily fall within the classification of major depression. For example, patients with bipolar disorder will present with symptoms of depression, but they are differentiated from MDD due to the presence of manic, hypomanic, or mixed episodes
Postpartum / antepartum depression
In a systematic literature review, more than 1 in 10 previously healthy mothers with no prior history of depression demonstrated symptoms of postpartum depression. Although less common, men can also suffer from postpartum depression.
Although a number of groups worldwide have determined elevated levels of anxiety and depression among pregnant women during the COVID-19 pandemic, a cohort study of women giving birth in Israel during the pandemic showed no evidence of an increased risk of MDD.
Some risk factors for postpartum depression can include:








Psychotic depression
A 2018 systematic review and meta-analysis reported a lifetime prevalence of 0.35–1%, with a similar gender distribution as MDD. Patients often present with more severe illness and have a longer duration of hospitalisation compared to non-psychotic depressive patients. Limited research into risk factors has identified a family history of psychosis and bipolar disorder.
Seasonal affective disorder (SAD)
SAD usually occurs during months with low sunlight and patients report:






To learn more about the symptoms of depression and how to diagnose MDD, visit the ‘Diagnosis and Symptoms’ page.
Abbreviations
ACNP, American College of Neuropsychiatry. DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. ED, Emergency department. ER, Emergency room. HAMD-17, Hamilton Depression Rating Scale. ICD-10, International Classification for Diseases, 10th Revision. MDD, Major depressive disorder. SAD, Seasonal affective disorder.